In June 2024, exactly one year after my sixth and final balloon pulmonary angioplastyBalloon Pulmonary Angioplasty Balloon pulmonary angioplasty, or BPA for short, is a technique for widening narrowed or blocked blood vessels in the lungs of CTEPH patients. Small balloons attached to a catheter restore blood flow to areas of the lungs that do not receive blood due to the disease. When successful, BPA eliminates or reduces shortness of breath, increases exercise tolerance and quality of life, and extends life expectancy. (BPABalloon Pulmonary Angioplasty Balloon pulmonary angioplasty, or BPA for short, is a technique for widening narrowed or blocked blood vessels in the lungs of CTEPH patients. Small balloons attached to a catheter restore blood flow to areas of the lungs that do not receive blood due to the disease. When successful, BPA eliminates or reduces shortness of breath, increases exercise tolerance and quality of life, and extends life expectancy.), I visited Okayama Medical Center (OMC) for the recommended routine checkup. The right heart catheterization (RHC) showed that I am cured. No more CTEPHChronic Thromboembolic Pulmonary Hypertension CTEPH is short for chronic thromboembolic pulmonary hypertension, a rare form of high blood pressure in the lungs caused by blood clots or narrowed blood vessels. High blood pressure in the lungs is often also called pulmonary hypertension.!
Back to normal
Following a total of six BPA procedures, my hemodynamic parameters are back to normal levels. There are no more signs of pulmonary hypertensionPulmonary Hypertension (PH) High pressure in the blood vessels leading from the heart to the lungs is called pulmonary hypertension. The arteries in the lungs and the right side of the heart are affected by pulmonary hypertension. If untreated, the right side of the heart will weaken over time, eventually leading to heart failure and death. The WHO has defined five distinct groups of pulmonary hypertension, each with a different cause. CTEPH is a form of PH (WHO group 4). - References: mayoclinic.org and cdc.gov. My mean pulmonary artery pressure (mPAP) is 20 mmHg, and my pulmonary vascular resistance (PVR) is 1.8 WU at rest. Based on the current definition of Chronic Thromboembolic Pulmonary HypertensionChronic Thromboembolic Pulmonary Hypertension CTEPH is short for chronic thromboembolic pulmonary hypertension, a rare form of high blood pressure in the lungs caused by blood clots or narrowed blood vessels. High blood pressure in the lungs is often also called pulmonary hypertension. (CTEPH), this data indicates that I am cured of the disease [1].—They didn’t check my pulmonary artery wedge pressure (PAWP) during my recent RHC. It wasn’t necessary, given my normal mPAP and PVR.

Between October 2022 and June 2023, I underwent a total of six BPA procedures at Okayama Medical Center (OMC), Japan (all conducted by Dr. Hiromi Matsubara): four in October and November 2022 and two additional BPAs in June 2023. In June 2024, one year after the sixth and last BPA, I went back to OMC for a routine checkup. Among other tests, we performed a right heart catheterization (RHC).
Read the story of my 2nd BPA procedure here.
After CTEPH diagnosis in Feb 2022, we started medical therapy with sildenafil and changed anticoagulation from edoxaban to warfarin. Edoxaban, a direct oral anticoagulant (DOAC), had been prescribed upon discharge from the hospital following multiple pulmonary embolisms. This post here contains a full timeline of events.
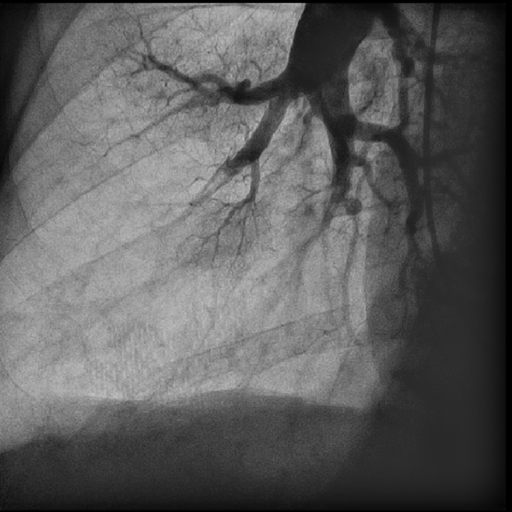
Radiographic images
These powerful radiographic images show how my lower right lung looked before and after BPA treatment. The difference between disease and cure is prominently visible—no need to be a physician to spot it.

Some limitations remain
While these hemodynamic parameters are within normal limits, it does not mean that my lungs operate at full capacity. Due to a few remaining minor obstructions, regional ventilation-perfusion (V/Q) mismatches still exist in my lungs. While air reaches these regions, insufficient blood flow prevents gas exchange (oxygen uptake and carbon dioxide release).
Since my hemodynamic parameters are back to normal, there is no need for additional procedures or specific medication other than blood thinners to prevent new blood clots from forming.
These V/Q mismatches don’t bother me in my daily activities. But when I work out hard, charging up steep hills, my blood oxygen levels (SpO2Blood Oxygen Saturation (SpO2) The oxygen saturation (SpO2) of a person's blood is defined as a percentage of the maximum amount (100%) of oxygen it can transport. A healthy person's SpO2 percentage should be between 96% and 99%. - Source: What is oxygen saturation (SpO2)? What is the normal range for SpO2??. Retrieved 11 November 2022, from ihealthlabs.com) drop fast. My lungs can’t keep up with the high oxygen demand of my muscles when pushing hard.
Typical blood oxygen levels
To give you an idea of my blood oxygen levels, my SpO2 is between 95% and 98% when seated. SpO2 is between 91% and 93% during moderately intense exercise, like cycling. Seated at cruising altitude on commercial flights, my SpO2 ranges between 91% and 93%. SpO2 drops to around 88% during more vigorous exercise, and when I charge up a steep hill, it can go as low as 84%.
No issues with temporary SpO2 dips
I don’t experience issues with temporary low blood oxygen levels. As long as my SpO2 stays above 82%, I don’t feel dizzy or experience visual problems. Slowing down allows my blood oxygen levels to recover quickly, almost immediately. My doctor has assured me that as long as these drops are temporary, the disease will not return.
My heart has recovered
Along with my hemodynamic parameters, my heart has also recovered. My right heart is almost back to normal. After gradually increasing my training load, my heart can handle intense exercise without any issues, and my doctors have given me the go-ahead to push hard.
The future looks bright
Lucky me, I don’t have any other health issues (comorbidities), and according to one of my doctors, I can live out my life without worrying about premature death due to CTEPH. He even mentioned one of his patients who underwent BPA treatment more than 15 years ago and is still going strong at age 80-plus.
Hard historical data shows low chances of recurring occlusions (restenosis) after successful CTEPH treatment [2]. However, to be cautious and as recommended by the current pulmonary hypertension guidelines [1], I am on lifelong anticoagulation therapy with warfarin to help prevent any new blood clots from forming.
Additionally, I plan to return to OMC in four years for another checkup.
Uplifting others
I share my story, hoping it can inspire and uplift others facing similar challenges. Remember, a cure is possible with proper treatment and the right mindset.
Big Thank You
Let me express my heartfelt thanks to all my doctors for making my recovery possible! A very special thank you to Dr. Hiromi Matsubara for having had the courage to develop and refine BPA. My gratitude also goes out to all the early patients who served as guinea pigs for the evolution of modern BPA. Without all of you, I would never have survived this disease.
References
[1] Humbert, M., Kovacs, G., Hoeper, M. M., Badagliacca, R., Berger, R. M. F., Brida, M., Carlsen, J., Coats, A. J. S., Escribano-Subias, P., Ferrari, P., Ferreira, D. S., Ghofrani, H. A., Giannakoulas, G., Kiely, D. G., Mayer, E., Meszaros, G., Nagavci, B., Olsson, K. M., Pepke-Zaba, J., Quint, J. K., … ESC/ERS Scientific Document Group (2022). 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. European heart journal, 43(38), 3618–3731. https://doi.org/10.1093/eurheartj/ehac237
[2] Inami, T., Kataoka, M., Yanagisawa, R., Ishiguro, H., Shimura, N., Fukuda, K., Yoshino, H., & Satoh, T. (2016). Long-Term Outcomes After Percutaneous Transluminal Pulmonary Angioplasty for Chronic Thromboembolic Pulmonary Hypertension. Circulation: Heart Failure, AHA Journals. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.116.024201







Comments by Gregor